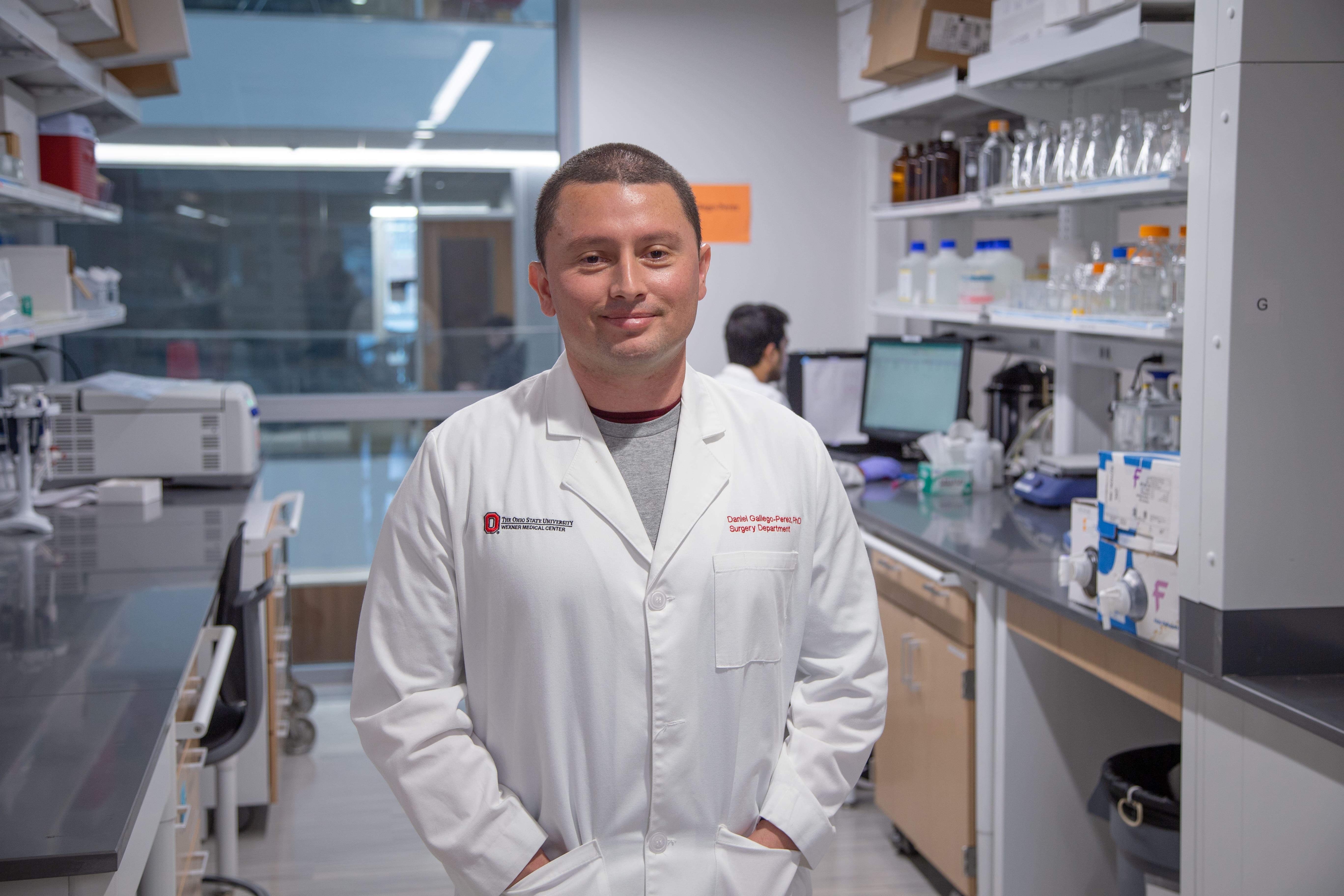
Gallego-Perez Laboratory
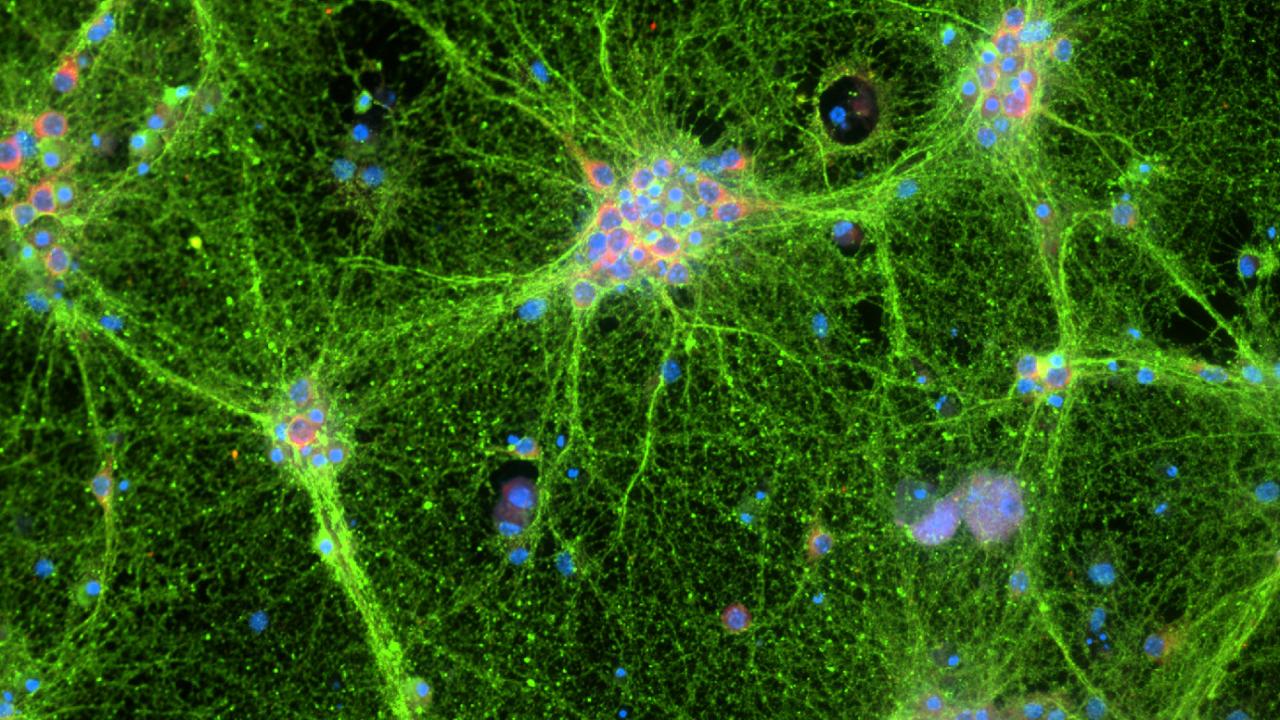
Dr. Gallego-Perez is widely recognized as an emerging leader in Biomedical Engineering, especially in the field of nanotechnologies for non-viral gene delivery, cell and tissue reprogramming, and regenerative medicine. In the past few decades, there has been a significant amount of research concerning methods for delivering genetic material to target cells with the intent to modulate their behavior. The applications of such technology are enormous for the treatment of different types of conditions, including trauma and/or degenerative disorders. However, current approaches to gene delivery rely primarily on engineered viruses as vectors for the genetic material. Viral delivery, while promising in some contexts, still faces a number of clinical difficulties. Dr. Gallego-Perez has made a number of substantial advances in the area of non-viral transfection through the use of nanodevices that will help overcome some of the obstacles associated with viral delivery. One of his most pivotal contributions to the fields of non-viral gene delivery and regenerative medicine involve the development of a nanotechnology-based platform technology, Tissue Nano-Transfection (TNT), to conduct non-viral genetic manipulations in vivo. This technological leap allowed Dr. Gallego-Perez and his team to explore the concept of “whole tissue” reprogramming, whereby complex multicellular structures can be genetically instructed to convert into a different type of tissue that could then be used to restore lost functionalities due to trauma or any other condition. Dr. Gallego-Perez was awarded the prestigious NIH New Innovator Award for his work on TNT and whole tissue reprogramming. The potential use of Dr. Gallego-Perez’s TNT technology has transcended beyond ischemic disorders in the skin and is now being actively investigated for the development of therapeutic interventions for peripheral nerve injuries (PNIs), as well as cutaneous and peripheral neurofibromas. The work on PNIs, in particular, which is currently being funded by the Department of Defense (DOD), has the potential to not only help active-duty US Servicemembers recover from a PNI more rapidly and effectively, but also decrease the incidence of severe and irreversible long-term consequences (e.g., pain, weakness, loss of independence, muscle loss, etc.) of PNIs in our veteran population. Moreover, with funding through NIDDK’s Catalyst Award program, Dr. Gallego-Perez and collaborators have been able to make significant progress towards controlling endocrine and metabolic function, from the skin, via TNT-mediated reprogramming of skin tissue into endocrine pancreatic tissue or brown adipogenic tissue (BAT). A stellar demonstration of the therapeutic potential of TNT for diabetes and metabolic disorders was recently published in Circulation, in which Dr. Gallego-Perez and collaborators showed that inducing BAT-like functions in the skin by TNT can promote weight loss and improved cardiometabolic health in preclinical models of obesity and metabolic disorders.
In addition to the New Innovator Award, Dr. Gallego-Perez’s contributions have been recognized with multiple other accolades, including the Cellular and Biomolecular Engineering Young Innovator Award from the Biomedical Engineering Society (2020), and the Distinguished Alumni Award from both his undergraduate alma mater (2021) and OSU’s College of Engineering (2020), just to name a few. Dr. Gallego-Perez also has a very strong funding record, bringing in approximately $10 million in extramural funding (NIH, DOD, private foundations), with $>8 million as the lead PI. Dr. Gallego-Perez has also published >70 research papers and 7 book chapters, with an H-index of 31.