Nervous System Diseases
The Burghes Laboratory is focused on understanding how reduced SMN levels give rise to Spinal Muscular Atrophy. Increasing SMN protein using gene therapy, small molecule drugs and antisense oligonucleotides ameliorates SMA in cell culture, mouse models and in humans. Yet, the particular function of SMN that is disrupted remains unknown. To study biological pathway altered by loss of SMN, the lab has used transgenic mice and cell culture to study proteins that are known to physically interact with SMN. This will give genetic evidence for the critical pathway and genes disrupted by SMN deficiency. Furthermore, the lab is using long range Nanopore sequencing techniques to study genetic variation in discordant SMA sibling pairs with identical SMN2 copy numbers. Bioinformatic pipelines and novel methods of variant analysis are used to identify of genetic modifiers of SMA severity in humans. Understanding the basic mechanism of SMA and SMN loss can lead to the identification of new therapeutic targets, which can then be tested in the Delta7 SMA mouse model and eventually translated to the clinic. In addition, the lab is developing next generation gene therapy for SMA through modification of the SMN2 gene using CRISPR technology. The Burghes Lab has expertise in the cloning of the SMN gene, transgenic mouse model creation, and the testing of therapeutics, including the development of gene therapy for SMA.ocuses on understanding genetic neuromuscular disorders on a molecular level. In particular, they are unraveling the molecular biology of spinal muscular atrophy (SMA). SMA is an autosomal recessive disorder that is characterized by destruction of motor neurons in the anterior horn of the spinal cord. The disorder is typically classified into three types based on clinical severity. SMA is caused by loss or mutation of the SMN1 gene, while the virtually identical SMN2 gene remains unmodified. The two genes essentially differ by a single nucleotide that affects the incorporation of exon 7 into the SMN message. As a result of this change in SM1, the SMN2 gene produces insufficient SMN protein for motor neurons. SMN supports the biogenesis of small nuclear ribonucleic proteins (snRNPs), which are essential for all cells. Currently it is not clear why high SMN levels are so critically important for motor neurons.
The researchers have developed a mouse model of SMA, which has shown that high copy number of the SMN2 gene can rescue the SMA mouse. They are using this model of SMA to understand why motor neurons are affected and to develop treatments for SMA. They are also using high throughput screening to look for compounds that can activate SMN, in the hope of finding new therapies for SMA.
The lab is also developing methods for treating Duchenne muscular dystrophy (DMD) using gene therapy. DMD is a muscle wasting disorder caused by mutations in the large dystrophin gene. They are particularly interested in strategies that use the adeno associated virus vector to deliver for gene therapy.
The Liu Lab develops next-generation genome editing technologies to create safe, effective, and clinically translatable therapies for genetic diseases. Their work focuses on discovering and optimizing new genome editing strategies, with applications to disorders of the liver, nervous system, and muscle.
Genetic diseases result from a wide range of mutations - point mutations, insertions, deletions, and chromosomal rearrangements - each representing unique therapeutic challenges. To address these, the Liu Lab is expanding the molecular toolkit for precise correction of disease-causing mutations and investigating how different cell types and DNA repair pathways influence editing outcomes.
In pursing these goals, they employ both viral and non-viral systems to deliver genome editors in vivo, enabling the evaluation of new technologies in disease-related contexts. By combining tool discovery, mechanistic insights, and practical applications, the Liu Lab aims to establish versatile platforms for durable genome editing-based therapies.
Dr. Russell Lonser's laboratory is a translational neuroscience group. They have developed several clinical programs based on MR-guided delivery of gene therapy and their translational efforts led to the initiation of four clinical trials in different neurological disorders (Parkinson’s disease and AADC deficiency) and brain tumors (brain stem glioma and glioblastoma). Currently, they are also developing new treatments for adult and pediatric neurologic and neurodevelopmental disorders such as Alzheimer’s disease, Huntington’s disease, multiple system atrophy and lysosomal storage disorders as well as for substance abuse disorders. As a part of the overall gene therapy platform, they’ve also developed devices and procedures to advance intracranial AAV-based gene therapies, cell therapies and drug delivery for neurological disorders and brain cancer for first-in-human clinical trials.
As a Research Scientist in the Lonser Lab, Dr. Jerusha Naidoo serves as the regulatory and clinical development lead for trials conducted by the Bankiewicz and Lonser groups.
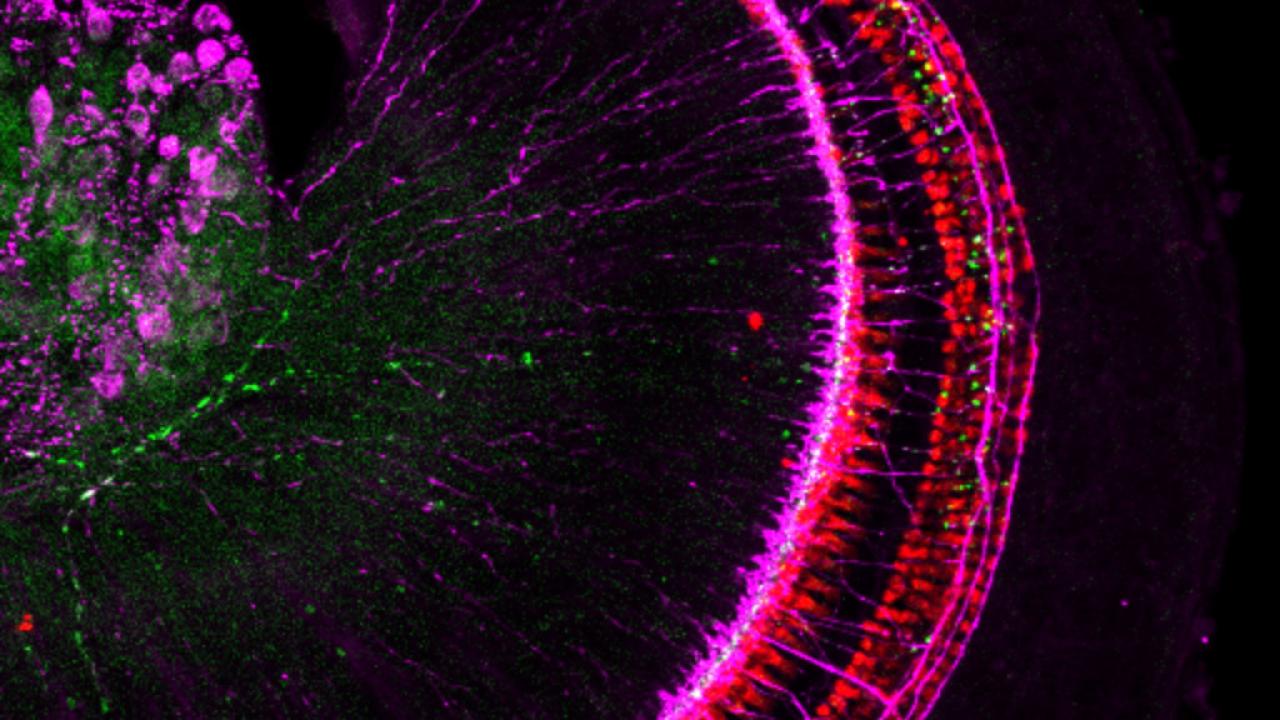
As a Research Scientist in the Lonser Lab, Dr. Victor Van Laar’s research focuses on understanding the role of mitochondrial dysfunction, cellular bioenergetics, and neuronal homeostasis in neurodegenerative diseases and other neurologically related disorders, including Parkinson’s disease, substance abuse, and depression. His research utilizes rodent models to better understand why these neurological conditions develop and how they might be treated. By developing and utilizing novel approaches for the delivery of therapeutic agents to target specific regions in the brain, Dr. Van Laar is also exploring gene therapy approaches to treating these brain disorders. Gene transfer and gene editing therapeutic approaches in the brain are evaluated by a combination of behavioral assessments and biochemical assays to evaluate efficacy. Techniques including immunohistochemistry, microscopy, quantitative image analyses, HPLC, and protein chemistry are utilized to assess the translational relevance of potential gene therapies.
The Gleichman Lab studies astrocytes as gene therapy targets for brain repair after stroke and in vascular dementia, two forms of ischemic brain injury. Astrocytes, one of the most prevalent cell types in the brain, can drive many of the processes needed to promote brain development as well as brain repair after injury. These cells also respond dramatically to an ischemic injury, walling off the damaged area and changing their functions in the spared tissue. We use mouse models to study how astrocytes respond to ischemic injury and identify points of intervention. In order to take advantage of those points of intervention, we are also developing ways to target astrocytic subpopulations with gene therapy, altering AAV expression profiles through the use of different capsids, promoters, enhancer elements, and miRNA targeting.
Dr. Herson’s research focuses on understanding mechanisms of injury and repair following ischemic brain injury, with studies related to ion channels/receptors, neuroinflammation, age and gender. Current studies are focused on the impact of ischemia on synaptic function and plasticity with the goal of revealing pharmacological interventions that both prevent acute ischemic injury and improve long-term brain function after injury. He received several NIH, DoD and AHA grants and has been continuously NIH funded throughout his independent career. Dr. Herson has published over 100 peer reviewer articles, developed multiple patents and mentored several junior faculty, both PhD and clinician-scientists.
The Kolb Lab is devoted to the understanding of molecular pathways that, when altered, result in diseases of the motor neuron. They are particularly interested in alterations in RNA metabolism that result in neurological diseases. The molecular mechanisms of spinal muscular atrophy and of amyotrophic lateral sclerosis (ALS) are current foci for biochemical and cell-based investigation. Their long-term goals are to determine the precise mechanisms that cause motor neuron diseases, including sporadic amyotrophic lateral sclerosis, and to develop small molecule and/or gene-based therapies for these diseases.
The Orfila laboratory focuses on understanding mechanisms of injury and repair following Traumatic brain injury (TBI), a leading cause of mortality and morbidity in adults, with significant sequelae including memory deficits. Despite intense research, no pharmacological interventions are currently available to improve functional recovery following TBI. The Orfila lab currently investigates the effects of TBI on memory acquisition and retrieval in a gender and age dependent manner. Through electrophysiological, behavioral and molecular methods, these studies focus on investigating the important cellular mechanisms underlying impaired hippocampal function, an area known for memory storage and retrieval. To advance their findings from mechanism to translation, they are using viral-mediated gene therapy as therapeutic strategies targeting pathways identified in their basic animal studies.
Breathing is a fundamental motor behavior required for survival, yet it is highly susceptible to disruption across a wide range of neurological diseases and injuries. The Rana Lab studies the neural control of breathing, focusing on how distributed brainstem and spinal cord circuits generate and adapt respiratory motor output, and how dysfunction in these circuits contributes to morbidity and mortality in neurological disorders.
A central emphasis of our work is respiratory dysfunction following spinal cord injury, where impaired breathing remains the leading cause of long term complications and death. Although current clinical strategies such as mechanical ventilation, respiratory muscle training, and diaphragm pacing can provide supportive care, they often fail to restore endogenous respiratory motor control. This highlights a critical need for therapeutic approaches that directly target the neural substrates underlying breathing. Beyond spinal cord injury, the Rana Lab investigates respiratory motor dysfunction as a shared and underrecognized feature of many neurological conditions, including amyotrophic lateral sclerosis, Rett syndrome, Pompe disease, aging-related respiratory muscle sarcopenia, and other neurodegenerative and neuromuscular disorders. We are particularly interested in defining common and disease specific mechanisms of respiratory circuit failure, to identify broadly applicable strategies to preserve or restore breathing across disease states.
Our research program integrates systems-level neurophysiology with therapeutic development. We employ in vivo respiratory neurophysiological recordings in awake and anesthetized animal models, noninvasive spinal neuromodulation, targeted pharmacological interventions, and rehabilitation-based paradigms designed to engage activity-dependent plasticity. A major and expanding focus of our lab is the use of gene therapy to develop optogenetic and chemogenetic tools that enable precise manipulation of respiratory motor circuits. These approaches allow us to address fundamental mechanistic questions regarding circuit organization and plasticity, while simultaneously informing the development of next-generation therapeutic strategies.
Yin Ren, MD PhD is a surgeon-scientist and an Assistant Professor in the Department of Otolaryngology . The Ren laboratory focuses on understanding the mechanism of tumor growth and extracellular matrix remodeling in diseases of the nervous system, particularly tumors of the cranial base such as vestibular schwannoma. Despite tremendous disease morbidity, no FDA-approved pharmacotherapies currently exist. Using cellular and animal models and tumor samples from patients undergoing surgery, the lab investigates molecular mechanisms underlying cellular proliferation and symptoms such as hearing loss. The laboratory is also developing nanotechnology-based tools to improve the diagnosis and targeted treatment of these tumors. Finally, in collaboration with investigators at the GTI and NCH, they are investigating AAV-mediated gene therapy as a therapeutic strategy for vestibular schwannoma and Neurofibromatosis Type 2. Dr. Ren also takes care of patients with hearing loss and skull base tumors at The Ohio State University Wexner Medical Center.
At the Samaranch Laboratory, we are committed to developing cutting-edge gene therapies for inherited disorders using recombinant AAV-based technology. Our core strength lies in the precise direct delivery of therapeutic agents into the central nervous system. We use stereotactic and microsurgical techniques, including intracranial convection-enhanced delivery, cerebrospinal fluid injections, and in-utero gene transfer. Our research includes capsid development, cell targeting and axonal transport optimization, and immune response assessment to provide disease-specific gene transfer needed to maximize the efficacy and safety of these treatments.
Our current preclinical studies include the therapeutic development for lysosomal storage disorders (Niemann-Pick Type A and GM1 gangliosidosis), neurotransmitter-related diseases (AADC and MAO deficiencies), and neurodegenerative diseases (Parkinson's and Alzheimer's diseases).
The Townsend Lab for Neurobiology & Energy Balance investigates how the nervous system (brain and peripheral nerves) regulate appetite, energy expenditure, and metabolic health. To do this, we take a broad physiological approach ranging from basic neurobiology to translational/clinical experimentation, encompassing neuroscience, cell and molecular biology, biochemistry, and metabolic physiology approaches using cell culture, mouse transgenic models, and human tissue samples. Lab projects fall in two areas of focus: 1) brain/hypothalamic adult stem cells and neural plasticity in the regulation of energy balance homeostasis; and 2) brain-adipose neural communication and adipose innervation by sensory and sympathetic nerves, including neurovascular and neuroimmune interactions, neurotrophic factor action, and adipose neural plasticity and neuropathy. Our research program impacts the study of obesity, diabetes, cardiovascular disease, cancer, and aging. Gene therapy projects include targeting peripheral nerves, adipose tissue, and the hypothalamus in the improvement of metabolic health and neural plasticity/remodeling.
As a Research Scientist in the Townsend lab, Dr. Magdalena Blaszkiewicz’s research program focuses on adipose neuropathy and potential gene therapy treatments, as well as neuroimmune interactions in the maintenance and control of adipose axonal health and plasticity. Her future independent research will focus on investigating how lymphatic vessels and lymph nodes in adipose serve as a nexus of neuroimmune cell crosstalk. A goal of this research is to determine if and how loss of nerves around lymphatic vasculature and lymph nodes in adipose tissues affect immune cell functions and trafficking, as well as fluid homeostasis in health and disease.